

Medical IDs for Lymphedema
A medical ID is recommended to anyone who is diagnosed or is at risk of lymphedema. Lymphedema is most commonly caused by the removal of or damage to lymph nodes as part of cancer treatment. When a person has lymphedema, it causes a blockage in their lymphatic system, leading to abnormal fluid buildup or swelling.
Patients diagnosed with lymphedema are at risk of severe complications like developing an infection or Lymphangiosarcoma, a rare form of soft tissue cancer. This is why a medical ID is recommended to anyone who has lymphedema or at risk of developing it. Wearing a medical ID can avoid serious complications by alerting responders, doctors, nurses, and other healthcare professionals of lymphedema.
There is no cure for lymphedema, but it can be managed by diligent care of affected arms or limbs.
"Consider buying a lymphedema medical alert bracelet that will help remind medical personnel which side to avoid for certain procedures." - TLC Direct, American Cancer Society
Avoid the following routine medical care on affected arms or limbs:
- Blood tests
- Blood draws
- Blood pressure checks
- Vaccinations
- IV injection
- Any procedure or test that involves needle insertion
These procedures may cause infections and lead to lymphedema symptoms for patients who have or are at risk of lymphedema.
“Avoid blood pressure cuffs, needle sticks, injections, or procedures on the affected limb. Wear a lymphedema alert bracelet.” – Vascular Cures
Who's at risk of Lymphedema?
Lymphedema can be primary or secondary. Primary lymphedema is a rare, inherited condition caused by Milroy's disease (congenital lymphedema), Meige's disease (lymphedema praecox), and Late-onset lymphedema (lymphedema tarda).
Secondary lymphedema is caused by any condition or procedure that impacted lymph nodes or lymph vessels such as:
- Surgery
- Radiation treatment for cancer
- Cancer
- Infection
Source: Mayo Clinic
Medical IDs and Lymphedema in Emergencies
In case of an emergency, wear a lymphedema medical alert bracelet or necklace. It's vital to inform medical healthcare professionals such as emergency responders, doctors, and nurses of lymphedema's presence or risk.
Any part of the body at risk of lymphedema is also at risk for severe and potentially life-threatening infection. Using medical id jewelry can communicate necessary lymphedema-related precautions to medical personnel, even if a patient cannot speak or become unconscious.
"A medical bracelet can let medical professionals know about risk for lymphedema. This may keep them from doing things that may make swelling worse." - Winchester Hospital
What to Engrave on a Lymphedema Medical ID
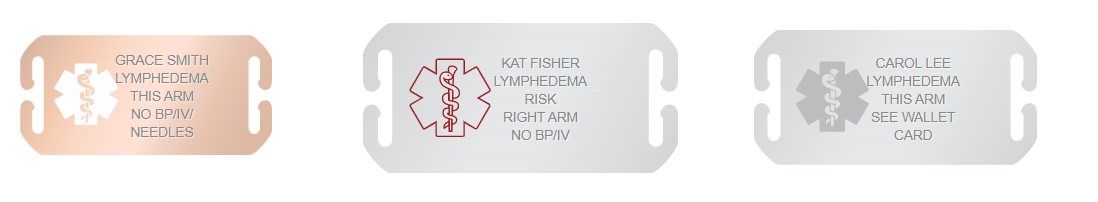
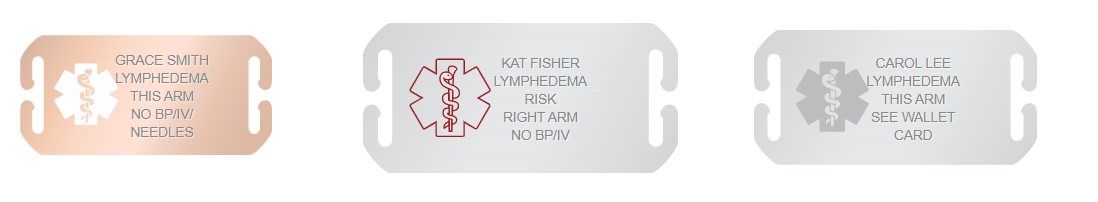
An emergency medical ID for lymphedema should quickly alert responders of lymphedema and the risk thereof. Personalized custom engraving can include necessary precautions and identify the affected arm or limb, as well as other medical conditions or allergies.
A lymphedema medical ID should include the following information:
- Name
- Lymphedema - identify affected arm or limb
- Lymphedema Alert - this arm
- Lymphedema Risk - right leg
- Lymphedema - this side
- Lymphedema precautions can be engraved as:
- NoBP/IV/Needles
- No blood pressure, no IV, no needles
- Right arm - no needles, no BP
- No needles or BP in this arm
- No needle, no bp on left arm
- Emergency contacts
- See wallet card - providing more information about lymphedema and other medical conditions can increase safety and peace of mind in emergencies. An expandable wallet card can hold more details such as additional guidelines and precautions that healthcare professionals should be informed of. A medical ID can direct responders to look and refer to an emergency wallet card for helpful medical information.
"If you have lymphedema, you may want to wear a lymphedema alert bracelet. These bracelets are worn to protect people who have lymphedema from receiving treatment such as blood pressure readings, injections, or blood draws to their affected limbs. These treatments could make their conditions worse." - Michigan Medicine, University of Michigan

 - UK
- UK  - Canada
- Canada  - Australia
- Australia 